Your Health Unlocked Episodes
041: Menopause Must-Knows in 2024 with the National Menopause Foundation
March 21, 2024
---
Consumer Health Info, Health Info
Publication Date: November 29, 2022
By: NWHN Staff

Osteoporosis treatment has radically changed in a relatively short period. In the early 1990s, women had few treatment options. Now, there are many different types of treatments available. This has created a dilemma for women trying to decide which, if any, of these medications they need. The NWHN believes that treatment should be focused on women who are known to be at high risk of fracture due to prior fractures, long-term corticosteroid use, or other known risk factors. Though drugs can be appropriate for women with severe osteoporosis who are at high risk of fracture, they are not the solution for everyone. Overall, efforts should focus on promoting bone health for all women and preventing fractures through various methods for those at risk.

We’ve developed this to help women understand what treatment options exist, the side effects and risks, what evidence supports their efficacy, and how to adopt non-drug approaches to preventing fracture. We hope this tool will help empower women to have conversations about osteoporosis with their providers, make informed decisions about whether they need drug treatment, and determine which drugs make the most sense for their unique circumstances.
Bisphosphonates are commonly prescribed for osteoporosis treatment and prevention. The FDA has approved many bisphosphonates to prevent bone loss and fractures in postmenopausal women: alendronate (brand name Fosamax), etidronate (brand name Didronel), ibandronate (brand name Boniva), risedronate (brand name Actonel), tiludronate (brand name Skelid), pamidronate (brand name Aredia) and zoledronic acid (brand names Reclast and Zometa). Some are taken daily; others are formulated for weekly, monthly, or yearly use. Bisphosphonates decrease the rate at which bone is destroyed, a process called resorption, by stopping the activity of the cells that cause bone breakdown, called osteoclasts. This slows down the rate of bone loss. The drugs are also incorporated into newly formed bone and can persist for years, so the effects last well beyond the final treatment.
The way bisphosphonates are prescribed has changed as our data has improved. The Network expressed strong concerns with the old “screen early, treat indefinitely” approach to osteoporosis that drug companies heavily promoted. This approach, which was routine in the 1990s and 2000s, led many healthy women to take bisphosphonates for long periods of time. In May 2012, the FDA expressed concerns about the safety and effectiveness of bisphosphonate use beyond five years. The agency told manufacturers to inform women that long-term use may not be beneficial. This advice was based on studies that showed women who took bisphosphonates for six or more years had higher fracture rates and suffered more complications than women who took bisphosphonates for three to five years.
Although many clinicians and pharma-sponsored education campaigns conflate prevention and treatment, the Network thinks that it is important for people considering bisphosphonates to understand how the effectiveness differs based on an individual’s bone health. These drugs have been shown to reduce the risk of a hip fracture in women who have been diagnosed with osteoporosis because of a previous fracture or very low bone density. However, they have not been shown to prevent hip fractures in women who have been told that they have osteopenia. They prevent vertebral fractures, including in women who have not previously fractured. Understandably, women may want to prevent vertebral fractures, which can be painful and debilitating. However, women should be aware that these drugs have side effects and rare but serious risks.
There have been numerous reports of unusual fractures in the thighbones of otherwise healthy women that took an inordinately long time to heal. Other women experienced severe bone, joint, and/or muscle pain. The FDA advises patients with such pain to consider discontinuing the drug, which usually causes the pain to go away. The jaw tissue of some women taking bisphosphonates dies (jaw necrosis), which can necessitate the removal of an area of the jaw bone. Bisphosphonates also can cause severe heartburn and ulcers and damage the stomach and esophagus if not taken in a very careful regimen (on an empty stomach, with a full glass of water, while sitting upright for up to thirty minutes).
For many years, the risks of bisphosphonates were unknown, and many healthy women who took these drugs experienced unnecessary side effects. We now have a much better understanding of the risk bisphosphonates pose and have a few strategies to mitigate them. We also understand which women will benefit most from treatment. For women who have already had a serious fracture and are looking to prevent a second or third fracture, the benefits of bisphosphonates may well outweigh the risks. For women with osteopenia who have never fractured, the Network seriously questions the benefit of bisphosphonate treatment.
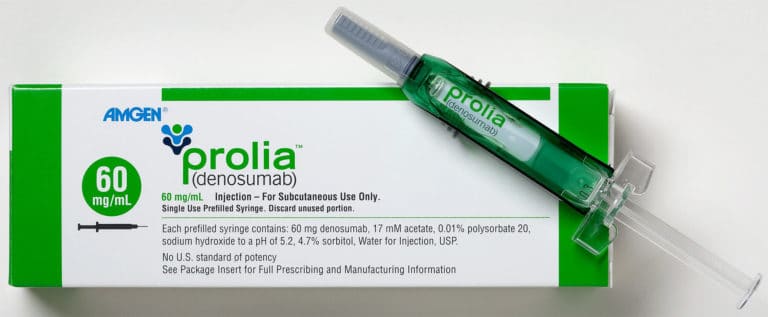 Denosumab (brand name Prolia) osteoporosis treatment medication (Amgen)
Denosumab (brand name Prolia) osteoporosis treatment medication (Amgen)
Denosumab (brand name Prolia) is an osteoporosis medication that uses human monoclonal antibodies. Approved in 2010, this drug works by targeting and inactivating osteoclasts to stop natural bone breakdown or resorption processes. Denosumab is given in a subcutaneous (just below the skin) injection twice a year. This treatment is intended for women with severe osteoporosis who are at high risk of fracture. For those women, a common first-line treatment plan will include two years of denosumab followed by three to five years of bisphosphonate use. This is because the fracture-preventing, bone-density-building benefits denosumab confers are quickly lost if not followed by several years of bisphosphonates.
Denosumab has proven effective at building bone density and reducing spine and hip fractures. However, it carries a risk of serious side effects. Denosumab’s cellular target in bone also exists in the immune system. This has led some women taking denosumab to experience serious infections requiring hospitalization (e.g., heart infections), making this a poor option for those with weakened immune systems. Since denosumab and bisphosphonates target the same biological pathways, it is unsurprising that denosumab also causes disintegration of the jaw, called osteonecrosis. It also may cause the same atypical femur fractures as bisphosphonates, though the causal relationship is less certain for this potential outcome. The treatment is also extremely expensive, costing thousands of dollars a year. Some insurance companies are reluctant to cover denosumab due to the very high price.
The Network is concerned that for most postmenopausal women, the benefit of denosumab does not outweigh the risks. We recommend that women seeking osteoporosis treatment approach denosumab with caution.
Two other hormones have been approved to treat osteoporosis: teriparatide and abaloparatide. Teriparatide (brand name Forteo) is a lab-made derivative of human parathyroid hormone (PTH), and abaloparatide (band name Tymlos) is a derivative of human parathyroid hormone-related protein. In the body, parathyroid hormone and parathyroid-hormone-related proteins stimulate the production of new bone tissue. The drugs mimic this activity. Both drugs are administered through injections into the fatty tissue, usually in the abdomen or thigh.
These drugs have been shown to stimulate new bone formation and prevent fractures in women with osteoporosis. However, the absolute reduction in fractures in clinical trials of these drugs was very small, between 2-4%. In addition to limited efficacy, these drugs have serious safety concerns. The drugs carry a label warning about bone cancer or osteosarcoma. This is because teriparatide caused bone cancer in animals during early testing. Other side effects include nausea, dizziness, leg cramps, dangerously high calcium levels, and vomiting. The recommended length of treatment for these drugs is two years; after this point, the effectiveness of the drug plateaus while the risks increase. It’s also very expensive, up to $19,500 annually, and some insurance companies are reluctant to cover it. Given the expense, the safety concerns, and the lower efficacy, teriparatide and abaloparatide are reserved for women with severe osteoporosis and are usually only prescribed when other treatment options have been deemed inappropriate or insufficient.
Menopause hormone therapy refers to the drug therapies of estrogen and progestin or estrogen alone that used to be routinely prescribed to women around the time of menopause. One of the justifications for practice was data showing that menopause hormone therapy could reverse bone loss and prevent hip fractures. However, the Women’s Health Initiative revealed that these hormones are dangerous. They increase the risk of breast cancer, heart attack, blood clots, and stroke.
Selective Estrogen Receptor Modulators (SERMs) are compounds that act like estrogen on some tissues (e.g., bone tissue) and have an anti-estrogen effect on other tissues (e.g., breast and sometimes uterine tissue). The FDA has approved raloxifene (Evista) to prevent and treat osteoporosis. Although raloxifene has been shown to reduce the risk of vertebral (spinal) fractures, it has no impact on hip or wrist fractures. The drug is also associated with serious risks, including life-threatening blood clots.
Although these medications used to be a relatively common treatment option for osteoporosis, we agree with the 2017 updated guidelines from the American College of Physicians that recommend against using either menopause hormone therapy or SERMs to treat osteoporosis.
Calcitonin (brand names Fortical or Miacalcin; not the same as calcium supplements) has been shown to prevent spine fractures but not hip and wrist fractures. It is approved to treat women with osteoporosis, but its approval was based on weaker evidence than more recently approved drugs, and its use is not generally recommended. Women who take calcitonin must watch their intake of foods with high calcium levels (e.g., milk, cheese) as excessive calcium can be dangerous. Calcitonin is administered through a nasal spray; side effects may include nasal congestion and nausea. Although calcitonin is technically still available, it is considered obsolete due to safety concerns and low efficacy compared to other treatments.

There are many ways to treat or prevent osteoporosis that do not rely on drug treatment. Though non-drug alternatives probably won’t replace drug treatment for women with serious osteoporosis, all women and men can take steps to build strong bones and prevent falls to reduce their risk of fracture.
It is vital to ensure your body has the nutrients it needs. This means getting the daily recommended dose of vitamin B, which has been linked to muscle health, and maintaining a healthy diet high in antioxidants. There are multiple ways to get the 700mg daily recommended dose of vitamin B. The nutrient is found in animal products like eggs, fish, poultry, and dairy and in some cereals, rice, and plant-based dairy alternatives.
Exercise is another critical way to maintain healthy bones. Studies have shown that exercise—especially weight-bearing regimens like walking, dancing, or running—increases bone density. Tai Chi – an ancient Chinese practice that combines slow, deliberate movements, breathing exercises, and meditation – has been shown to be one of the most effective exercise regimens for increasing bone density and reducing fracture risk. An added benefit of exercise is that it increases strength and balance, which can reduce the risk of falling, which leads to fracture.
Even the weakest bones are unlikely to break without some form of trauma. When an older adult breaks a bone, falls are often to blame. Falls contribute to over 95% of osteoporotic hip fractures. If you have been diagnosed with osteoporosis, reducing the risk of falls is an essential part of a comprehensive fracture-reduction strategy. Whether or not you choose to take medication, there are several methods to reduce your risk of falling and experiencing a fracture.
Making your home “fracture-proof” is an excellent place to start. Studies show that taking steps like taping down the edges of rugs or mats, installing textured pads to showers and slippery floors, ensuring good lighting – especially in stairways – and wearing stable nonslip shoes around the house successfully reduce the risk of fracture. When you leave the house, wear nonslip shoes and be aware of slippery surfaces, especially in the winter when walkways can be icy.
Consistent exercise, especially daily balance training, can help strengthen muscles that stabilize the body. Balance training exercises can be found online and done at home. Classes and programs also exist and may be advisable for those who are frailer. Poor vision can lead to tripping, slipping, and possibly fracture. Getting regular vision checks and using prescribed eyewear is also important.
Dizziness and fainting are common side effects of many drugs prescribed to older adults. Check the FDA label online or in the package insert to determine whether any drug you take can cause these side effects. Though you cannot predict how your body will respond to any given medication, taking the proper precautions, like sitting down when you feel dizzy or faint, can help you avoid falls. It is also good to schedule an appointment with your primary care physician once a year to review your medications. These appointments, called “brown bag” appointments, involve bringing all the medications you take to the appointment in a bag and talking with your physician about which prescriptions could be stopped or changed. The number of medications prescribed to older adults, especially those with chronic conditions cared for by multiple physicians, can be staggering and sometimes isn’t necessary. A brown bag appointment is not only a good health and safety measure, but it could also help lower the dosage or even eliminate drugs that cause dizziness or fainting.
Think carefully about your own risk of experiencing a serious fracture and consider safety issues when deciding whether to take osteoporosis drugs. Don’t hesitate to ask your health care provider about the safety and efficacy of osteoporosis medications and whether non-drug alternatives might be just as effective, based on your history and current health status. For more information, visit the National Institutes of Health Osteoporosis and Related Bone Diseases Resource Center’s website.
