
Your Health Unlocked Episodes
049: Ensuring Financial Health as We Age with The Senior Source
July 11, 2024
---

Deep Dive Articles
Publication Date: August 22, 2023
By: Interview Granted by Cindy McKendall, NWHN Member

Interview Granted by Cindy McKendall, NWHN Member
Edited by Adele Scheiber, NWHN Director of Communications
Menopause is defined by the National Institute on Aging as “A point in time 12 months after a woman’s last period.” The years leading up to that point, when women may have changes in their monthly cycles, hot flashes, or other symptoms, are called the menopausal transition or perimenopause.
Perimenopause most often begins between ages 45 and 55. It usually lasts about seven years but can be as long as 14 years. Cindy McKendall is just one of thousands of women who have lived for years with perimenopause. She is 48 and lives in Illinois with her husband and two teenage daughters. She works from home full-time and enjoys hiking, comedy, and reading. We found Cindy in a virtual patient support group and asked her to share her lived experience of perimenopause with our members. This is her story.
***This interview has been edited for length and clarity***
Sure. My name is Cindy McKendall, and I am 48 years old. I have been in what I believe is perimenopause for either ten years or six years, depending on which symptoms you go by. And part of the reason that I’m not sure how long it’s been is because I had a hysterectomy when I was 40, about eight years ago. I had a hysterectomy because I developed endometriosis after what I think was an estrogen surge in my late 30s. All of a sudden, my periods became very painful, and I tried a few different things, but luckily, I had a really good OBGYN who ultimately recommended the hysterectomy, which helped for a while. But in 2017, about two years later, I started having insomnia that was different from the lifetime of insomnia that I had dealt with before.

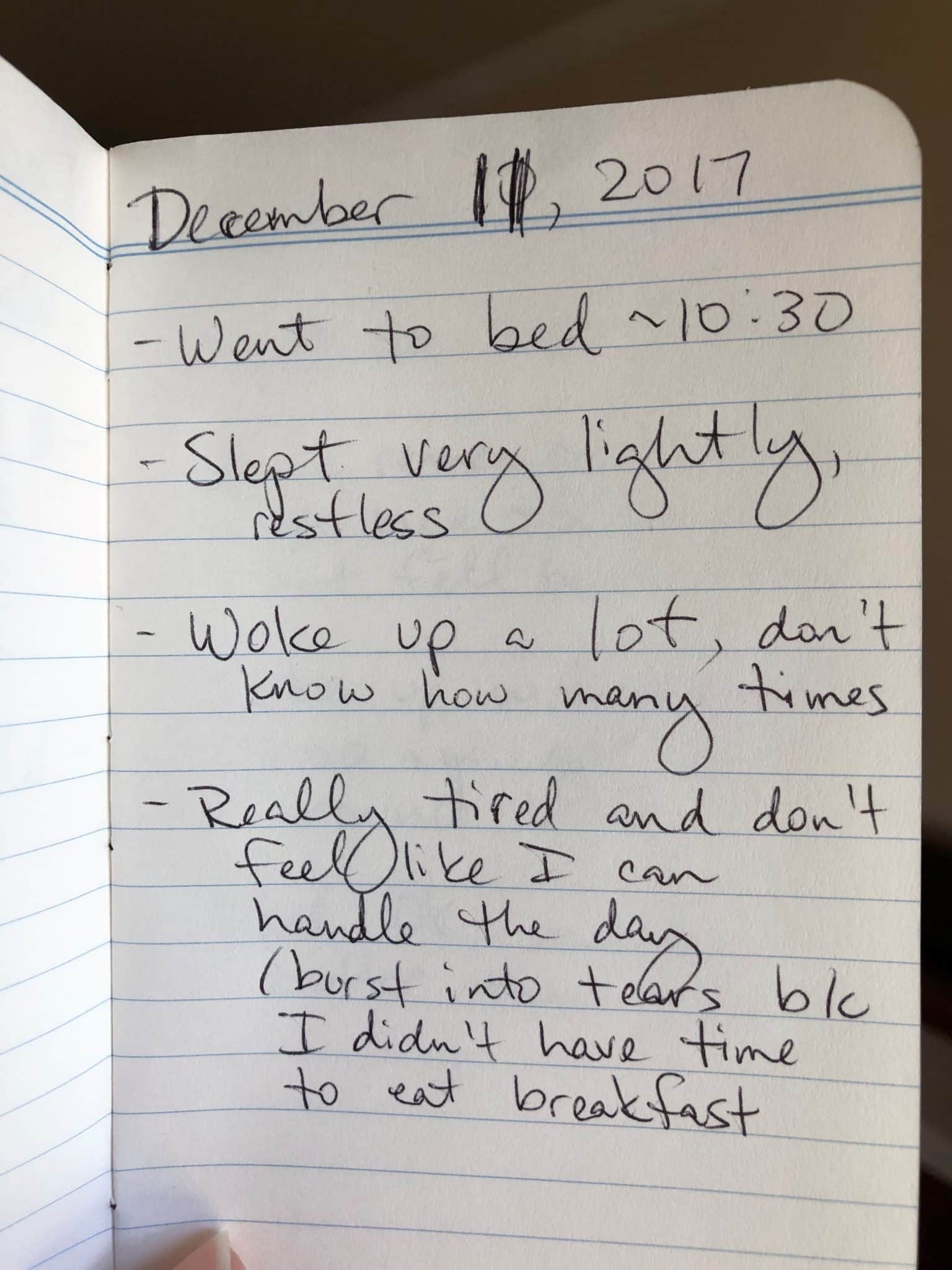
So, before, when I was younger, I always had difficulty falling asleep. Once I could fall asleep, which sometimes took up to an hour, I could sleep for, like, seven or eight or nine hours, and it was generally fine. In the fall of 2017, I started waking up in the middle of the night, so I would be waking up multiple times during the night, not getting an unbroken night’s sleep, and not feeling rested. And so, I kind of date that as my earliest perimenopause symptom, which is why I say it’s six years. But it could have been ten years if I go by the shortening of my cycle that I had before the hysterectomy.
Anyway, I kept a journal of my sleep symptoms in the fall of 2017 so I could take that to my doctor. Here is a pretty typical entry from that time period:
I went to my doctor pretty soon after that, and they recommended Melatonin, so I started taking it. That sort of worked for a while until it didn’t anymore. I also took a meditation class around that time to help with the anxiety that I was having, which I now know is another symptom of perimenopause. But at the time, I just thought it was because of everything going on and, also, I was in a toxic work situation which I ended up quitting in 2018. The meditation class was probably one of the more effective things that I’ve actually tried for my insomnia, but it still wasn’t getting me all the way where I needed to be.
In 2019, because the melatonin wasn’t really working for me, my doctor put me on an anti-anxiety medication called Effexor, and that did nothing for me. It made my insomnia worse. So I went off of it as soon as I could. And then, in 2020, that’s when the pandemic started, and everything got much worse in terms of my symptoms. I think stress probably exacerbated everything that was going on with my body. And not only was I waking up a lot, I was generally only sleeping a few hours a night. So, you know, waking up at four in the morning, and that was it for the night. So it really all came to a head in 2021 when it felt like things were getting better in terms of the pandemic and the world around us,
“but for myself and for how I was feeling, I was looking around and thinking-why don’t I feel better? If everything is getting better, why do I feel so terrible?”
In the fall of 2021, I think I was only sleeping like two or three hours a night. The week before Thanksgiving, I had a breakdown. I had a day where I tried to start my work day, and I couldn’t function. I started crying and couldn’t stop. I was supposed to call into a Zoom meeting, and I couldn’t do any of it. I just couldn’t stop crying. Luckily, I work from home and have a really caring boss who is actually a woman in her fifties herself. I was able to get a hold of my boss and say, I think I need some time off. She could tell by the sound of my voice that something was very wrong, but I didn’t have to explain it to her. I ended up taking about two weeks off. I got an emergency appointment with my doctor, who then put me on Celexa, which is an antidepressant.
It was all being treated as not connected. Providers would say, “Oh, you are anxious, so let’s treat your anxiety.” Never mind the fact that I’d never had symptoms of anxiety before. Same thing with the depression that I was experiencing. I have always been able to handle what life throws at me. I have experienced depression, but it tends to be situational and not chronic. So, this felt different than the times before when I dealt with depression.
Another factor that contributed to this fractured care, I think, was that my doctor was a little younger and didn’t have any personal experience with menopause. By that point, though, I’d started to understand the importance of educating and advocating for myself. I had read a couple of books about menopause, and that really helped me understand what the hell was going on with my body. I had also been reaching out to a lot of my friends, people my age, to ask them, are you having these same problems? I don’t understand what’s going on with me. Are you having the same thing? By and large, my friends were like, “I’m having a little bit of issues, but no, nothing like what you’ve got going on.”
A little bit, but it also had side effects. It made my stomach feel terrible, so I did not stay on it very long. When I went back to the doctor for a follow-up, I asked for hormone therapy, and she said she wasn’t familiar enough with the treatment risks and benefits to be comfortable prescribing it herself. But she was able to refer me back to my gynecologist, who had done my hysterectomy, had also delivered my kids, and is now a NAMS-certified menopause specialist.
“So I got really lucky in that respect that a doctor that I knew and trusted is also now a menopause specialist, and she’s also my age.”
When I went to her and had a consultation, she was very open to the idea of hormone therapy. So it was about a year ago, January 2022, that I started on an estrogen patch. Besides meditation, that has helped my insomnia more than anything. But I’m still waking up multiple times during the night, and I never feel rested and very rarely have energy.
The fatigue is very debilitating. I currently don’t have much of a life. I work from home and the energy that I have, I direct mainly just to my job and making sure my family gets fed. And then, I am a couch potato at the end of dinnertime, and I go to bed and sometimes try to tell myself I’m going to sleep great tonight and do some positive affirmations or whatever, but that doesn’t usually actually happen. I used to be someone who exercised regularly, and I miss that. I used to go see friends, and I don’t do that anymore. I really feel like I’m just existing and not living.
The anxiety and depression have improved drastically thanks to the estrogen. One of the insidious things about perimenopause that I’ve learned is that there are so many ways that hormones affect all the systems in your body, and nobody really teaches you any of it. You have to figure it out on your own. So that’s what I did. Things like, I had really dry, itchy skin for a while when I’ve always been oily. That was a perimenopausal thing that’s gone away with the estrogen patch. The anxiety was definitely one thing, brain fog is another thing. I still kind of struggle with verbal recall, but it is not as bad as before I started on estrogen.
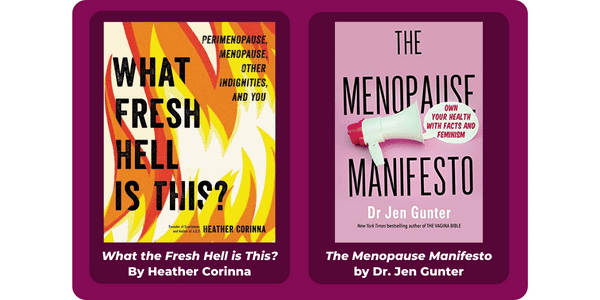
What I found most helpful was educating myself on what perimenopause is and what we can do about it. For me, that was through books because I’m a book nerd. I read a book called What Fresh Hell Is This? I found that really, really helpful in making the connection between what was going on in my body and the hormonal chaos that I was experiencing. It was very validating to know that I wasn’t going crazy. The other book I found helpful was called The Menopause Manifesto, which was written by an OBGYN named Dr. Jen Gunter.
Another piece of advice I have – try to find a provider who has really specific, specialized experience in your issue. One of the surprising things I learned throughout my journey is that most medical doctors get maybe an hour’s worth of education on menopause during their medical school training. When I told my doctor, “Hey, I think this is all due to perimenopause and want to go on hormones,” she told me flat out she didn’t have the knowledge to treat me – but to her credit, she admitted this and gave me a great referral.
Finally, I want anyone reading to know you’re not alone. Even if no one you know personally is experiencing these things or your doctor doesn’t understand. You can find community from the comfort of your own home. For instance, I found the menopause community on Reddit, which is where the NWHN reached out to me. And now, I get to be open about my story in the hopes it will help others. That’s really gratifying.
Our professional editing staff will work with you to make sure your contribution stands out. And don’t worry – we’ll take our lead from you on things like anonymity, important word choices, and accompanying imagery. Let us help you be seen, heard, and understood. Pitch us by filling out this short form, or just send us an email with your ideas at [email protected].
liked this page? Donate today!
The information on this site is not intended or implied to be a substitute for professional medical advice, diagnosis or treatment. All content, including text, graphics, images, and information, contained on or available through this website is for general information purposes only.
The continued availability of external resources is outside of the NWHN’s control. If the link you are looking for is broken, contact us at [email protected] to request more current citation information.
