Your Health Unlocked Episodes
050: Voting in 2024 – Why it Matters and How to Do It
July 25, 2024
---

Consumer Health Info, Health Info
Publication Date: November 11, 2022
By: NWHN Staff

A Hysterectomy is the surgical removal of the uterus that may involve removal of the cervix, ovaries, Fallopian tubes, and other surrounding structures. It may be done for a variety of reasons: Uterine fibroids, bleeding, Uterine prolapse and Cancer of the uterus, cervix, or ovaries.
Hysterectomy is the second most frequently performed surgical procedure (after cesarean section) for U.S. women who are of reproductive age. According to the Centers for Disease Control and Prevention (CDC), from 2006-2010, 11.7 percent of women between the ages of 40-44 had a hysterectomy [1]. Approximately 600,000 hysterectomies are performed annually in the United States, and approximately 20 million American women have had a hysterectomy [2]. By the age of 60, more than one-third of all women have had a hysterectomy. The NWHN believes that unnecessary hysterectomies have put women at risk needlessly and that health care providers should recognize the value of a woman’s reproductive organs beyond their reproductive capacity and search for hysterectomy alternatives before resorting to life-changing operations. Quoted in the Los Angeles Times, NWHN Executive Director Cindy Pearson says, “I advise any woman who is not in a life-threatening situation to see someone else besides a surgeon to explore nonsurgical options first.”
It may be a medically necessary procedure in the case of several life-threatening conditions:
If alternative treatment options (see “Hysterectomy Alternatives” section below) are not viable and a hysterectomy is necessary, it is important to initiate open communication with your health care provider regarding the specifics of your situation. Here are some important questions (adapted from The Woman’s Guide to Hysterectomy by Adelaide Haas and Susan L. Puretz) that you may want to ask your health care provider before you decide on a hysterectomy:
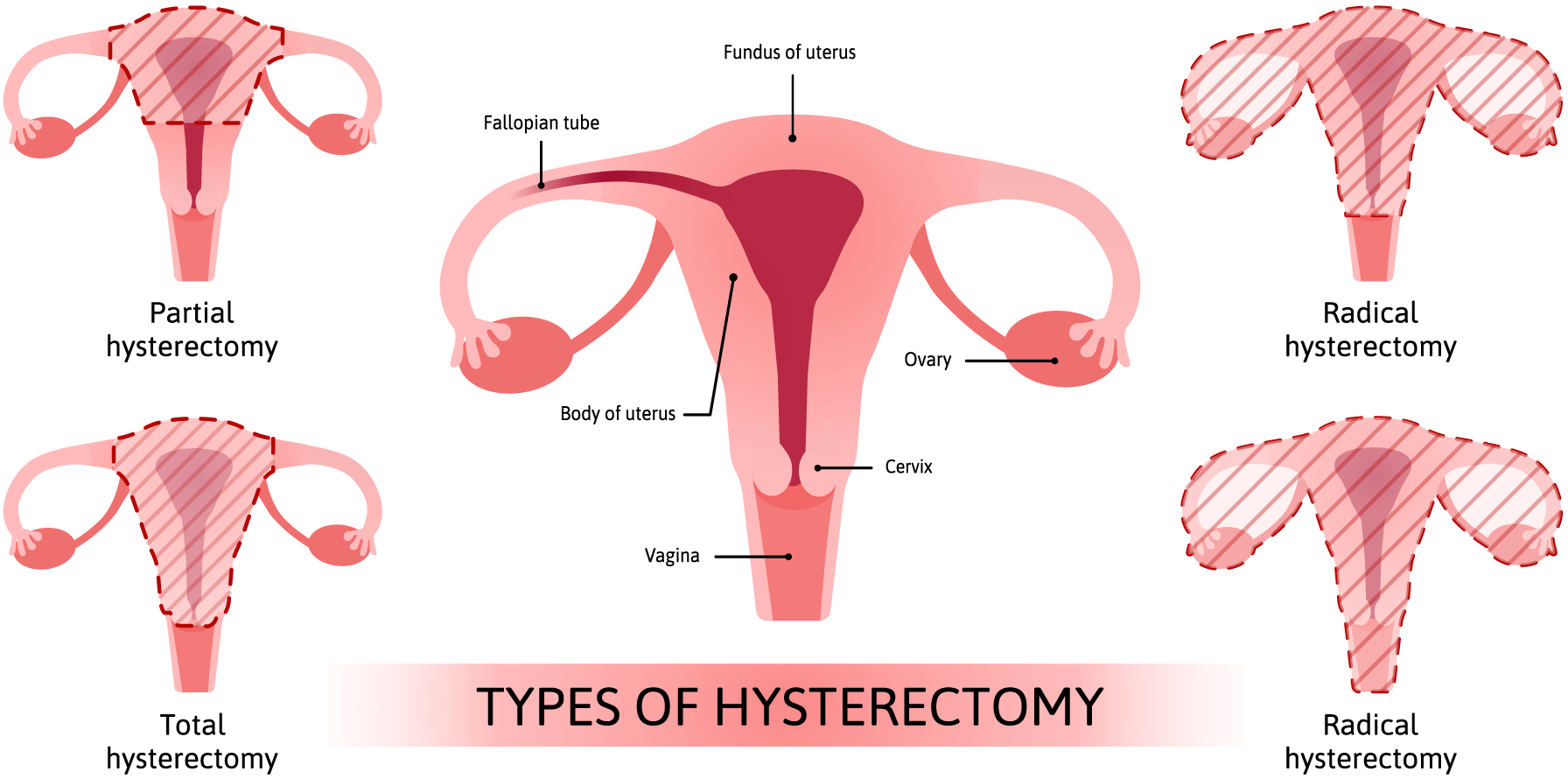
Your healthcare provider will discuss different potential surgical options for hysterectomies. You may have a hysterectomy performed as an in-patient procedure, or you may have a hysterectomy performed as an outpatient procedure. In 2008, approximately 18% of all hysterectomies were performed as same-day outpatient surgery [3]. Most of the research literature indicates that vaginal hysterectomies have better outcomes and fewer complications, but whether you can choose this procedure is dependent on feasibility and the condition for which you are being treated [4].
Although the death rate from a hysterectomy is low (less than 1 percent), surgical complications are very real and can result in any of the following: infection, hemorrhage during or following surgery, and/or damage to internal organs such as the urinary tract or bowel. Patients have a 30% chance of complication (typically infection or fever) while in the hospital and a significantly lower risk of more serious complications such as hemorrhage or bladder and bowel damage, depending on the individual’s condition and the surgical approach taken.
Removal of the uterus and ovaries at a young age (early forties and younger) may increase the risk of a heart attack, stroke, and (even when ovaries are not removed) the chances of experiencing an earlier menopause. Hysterectomy has also been associated with urinary problems, such as increased frequency of urination, incontinence, fistula, and urinary tract infections; sexual function problems, such as a decrease in sexual sensations and lack of lubrication; depression or psychological stress (stemming from feelings associated with losing reproductive organs); hormone deficiencies (which may be caused by removal of the ovaries), or a decrease in blood supply to the ovaries. There is not enough consistent evidence to know what the effects that a hysterectomy has on sexual function.
All four types of hysterectomies require the removal of the uterus. Therefore, once a woman receives a hysterectomy, she can no longer have a biological pregnancy in her own uterus. If the ovaries remain, she could utilize fertility treatments and have her eggs removed for fertilization and implantation in a surrogate.
For each of the conditions listed below, you may want to talk to your physician about an approach called “watchful waiting.” If your condition is not causing problematic symptoms, you may want to closely observe your symptoms without initiating active treatment. Many women are treated for conditions that do not necessarily require treatment, and the side effects of these treatments can cause more health problems than the actual condition. In many circumstances, you can carefully observe if and how the condition changes or is, hopefully, naturally eliminated.
There are many treatment options for shrinking or removing uterine fibroids without removing reproductive organs. These include using anti-estrogen drugs, uterine artery embolization (UAE) laser ablation of uterine fibroids, cryosurgery, and myomectomy. Read our Fibroids content for more information.
Hysterectomy is often necessary and life-preserving when invasive cancer is diagnosed; however, hysterectomy is frequently recommended when cancer is neither invasive nor life-threatening. For pre-cancerous cells, there are a few options that you and your health care provider should discuss. Loop Electrosurgical Excisional Procedure (LEEP) can be used to remove pre-cancerous cells, and cryosurgery can be used to treat non-cancerous growths and abnormal tissue. For early invasive cervical cancer that has not spread to other regions, a radical trachelectomy (the removal of the cervix or the neck of the uterus) can be performed in lieu of a total hysterectomy.
Endometrial ablation can be used to remove the excess endometrial lining. Dilation and Curettage (D&C) can also be used to remove the lining or abnormal tissue.
Operative laparoscopy is a surgical procedure that can generally be done on an outpatient basis to remove endometrial growths and adhesions. Pain medication, hormone therapy, and other conservative surgical procedures can also be used to control any discomfort associated with endometriosis. Read our Endometriosis content for more information.
According to MedlinePlus, an information service of the National Institutes of Health (NIH), a vaginal pessary (an object inserted into the vagina to hold the uterus in place) can be used as a temporary or permanent form of treatment for a prolapsed uterus (MedlinePlus). Vaginal pessaries are available in many shapes and sizes and must be individually fitted. A surgical procedure called a “suspension operation” can also be performed to lift and reattach a descended uterus and often a fallen bladder or rectum as well. Health practitioners suggest that Kegel exercises can be a powerful prevention and treatment tool for strengthening uterine muscles and avoiding prolapse.
Often, when getting a hysterectomy, doctors might suggest removing the ovaries to prevent ovarian cancer down the road. This, however, is not always medically necessary unless you are at risk for ovarian cancer or have a family history of ovarian cancer. While removing the ovaries does eliminate the risk of ovarian cancer, it may contribute to increased risks of heart disease and death. According to Our Bodies, Ourselves, ovarian cancer accounts for 14,700 deaths per year in the United States, but heart disease accounts for considerably more at 326,900 per year, and strokes cause 86,900. Conserving the ovaries during a hysterectomy should be carefully considered based on personal medical history and should be discussed with a physician before opting for removal.
References
