By: Carter Ringo
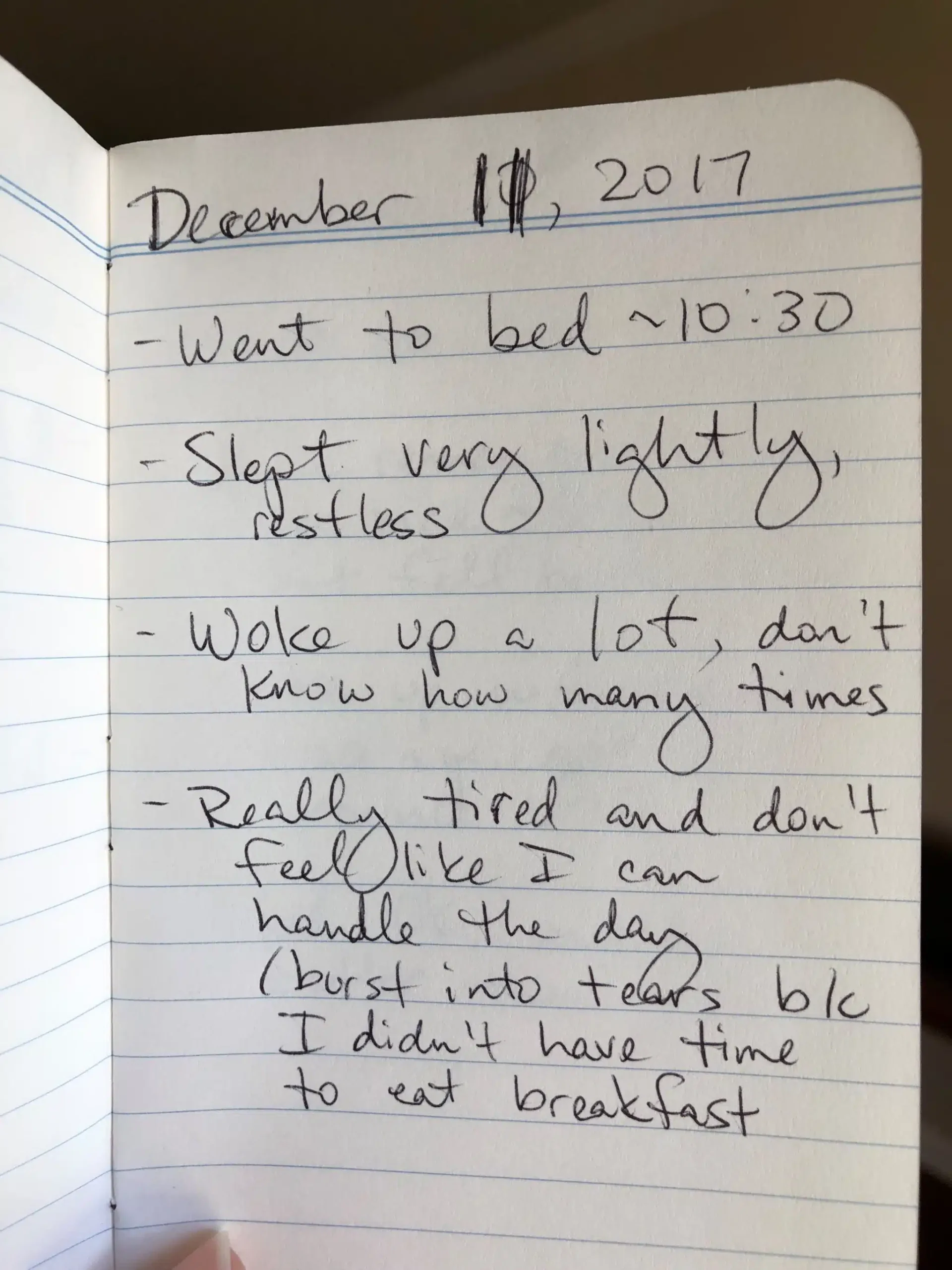
First thing every morning, I do a full body check. I check to see if any of my joints are out, whether my heartbeat is normal, and what my mental state and energy level is like. If I wake up with palpitations, it’s back to bed. If my joints are dislocated, I reset them myself or just continue my day hoping they will reset on their own at some point. The chronic pain, careful energy regulation, and gender dysphoria are just everyday facts of life.
My name is Carter, and I am a disabled nonbinary feminist. I was diagnosed with Hypermobile Ehlers Danlos Syndrome (hEDS) in 2014, and there are a few things about my life and my people I’d like to share with you.
1. hEDS is a rare genetic disorder, and a large percentage of the population with hEDS also identifies as having gender dysphoria like me[1].
Mainly, it affects collagen and soft tissue formation throughout the body. Collagen is a protein found in connective tissues, and connective tissues are what holds your body up and in. Connective tissues keep your organs in place, your skin strong, and your joints in socket. Connective tissues are like rubber bands that support your body into the form it is meant to be in, but an EDS-ers body’s rubber bands are filled with holes. We all know what happens to rubber bands with holes in them: when stretched too far they snap, and over a long time they become loose. Every day I dislocate multiple joints, most often my wrists, hips, fingers and toes. That may sound very bad, but for me at least minor dislocations are just inconveniences. I’m used to it and know how to take care of myself.
2. At 14 years old, I was told that I would be profoundly disabled for the rest of my life.
That was eight years ago. Being disabled is just the reality of living with hEDS. The hypermobile kind of Ehlers Danlos syndrome is considered the “mildest” medically, even though co-morbidities include POTS, Mast-cell activation syndrome, gastroparesis, chronic fatigue, depression, anxiety, widespread generalized muscular pain, and more. I have quite a few of these, and my mobility ranges day to day. However, I am proud that I exist with, and not despite, my disabilities. I have a strong support system and identify with the disabled community. I am also an accomplished artist and advocate, with an amazing partner and cat.
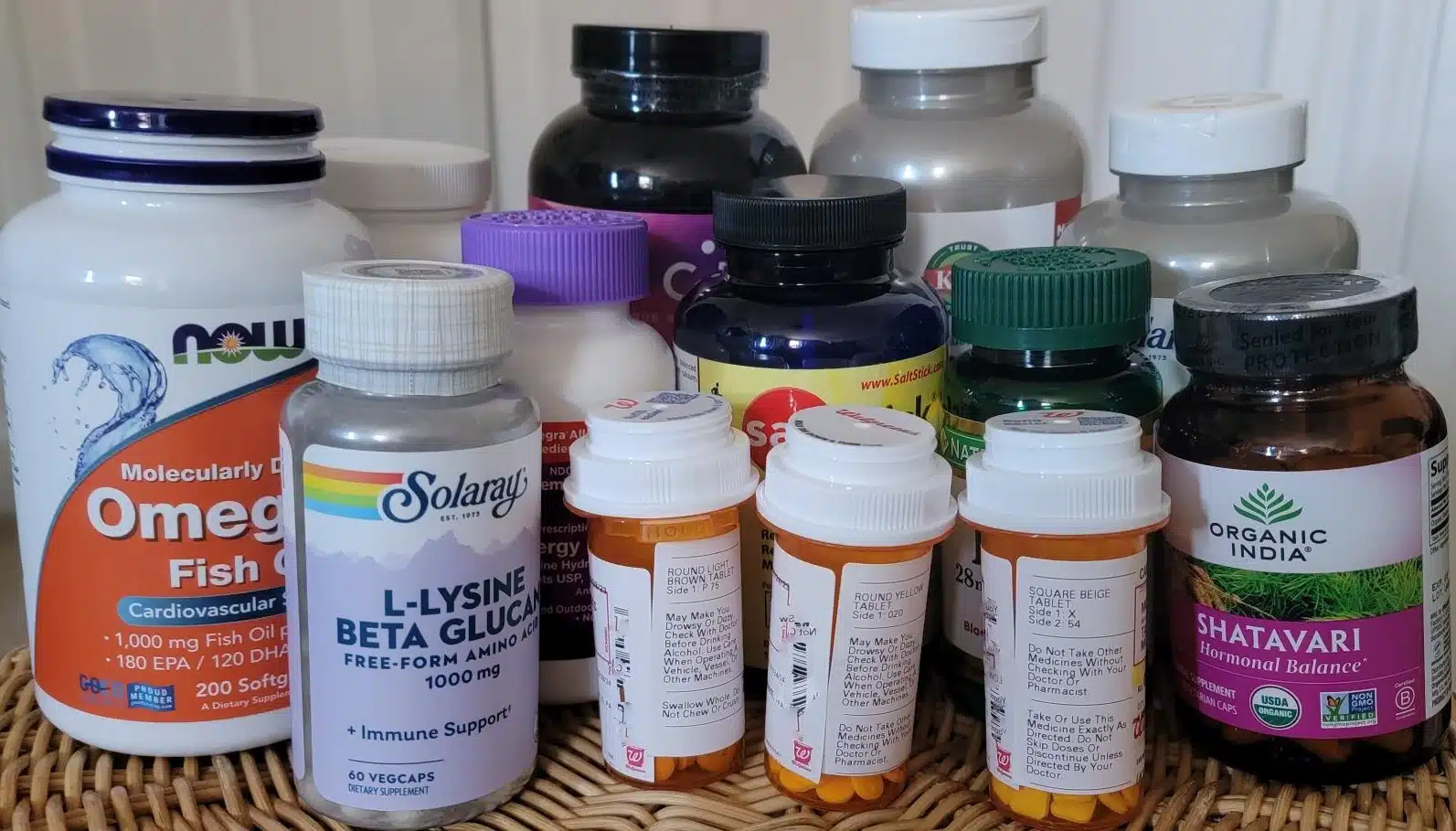
3. A strict treatment regimen rules my schedule (and my bank account).
Migraine rescue pills, muscle relaxers, pain medication, and a thousand or so supplements make up my day-to-day and a large percentage of my budget. Depending on insurance, these costs can add up to hundreds of dollars per month. Furthermore, the instability in my ribs prevents me from binding my chest and expressing as the gender I identify with, but I find other ways to outwardly signal my trans-masculine identity. I have also had to learn to perform and succeed at a much faster pace than others, because I know there may be a symptoms flare that leaves me bedridden for weeks, in need of intensive interventions, or even hospitalization.




 These organizations provide accessible, expansive, culturally congruent care and services with focuses ranging from community wellness, prenatal care, doula and lactation services, mental health and wellness, sexual and reproductive health education, and reproductive justice advocacy.
These organizations provide accessible, expansive, culturally congruent care and services with focuses ranging from community wellness, prenatal care, doula and lactation services, mental health and wellness, sexual and reproductive health education, and reproductive justice advocacy.